Uterine Prolapse
Uterine Prolapse
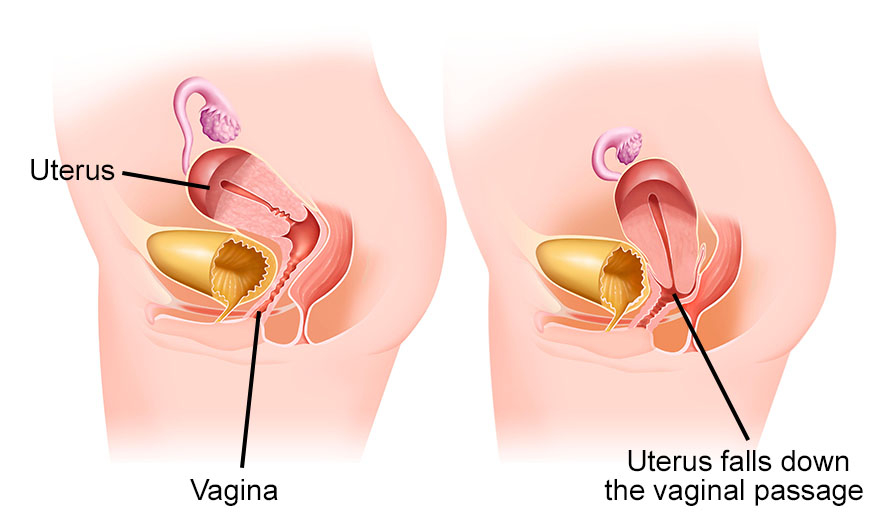
The uterus is kept in position by pelvic muscles and ligaments. Stretching of the pelvic floor muscles and ligaments causes uterine prolapse. As a result, the uterus sags slips into or protrudes from the vagina.
Uterine prolapse can be either complete or incomplete. Complete prolapse occurs when the uterus falls significantly and some tissue protrudes outside of the vagina, whereas incomplete prolapse occurs when the uterus is only partially drooping down the vagina.
There is no age limit for uterine prolapse. It can affect women of any age. However, it is more common in postmenopausal women who have had one or more vaginal deliveries
Uterine prolapse symptoms
- Tissue protruding from your vagina
- Urinary problems or frequent urination
- Difficulty having a bowel movement
- Feeling some pressure in the pelvis
- Generally, symptoms are less bothersome in the morning and worsen over the day. If the signs and symptoms of uterine prolapse interfere with daily activities, it is essential to seek medical advice.
Causes of Uterine prolapse
Uterine prolapse is caused by a weakening of the pelvic muscles and supporting tissues. Let’s look at what causes pelvic muscle and tissue weakness.- Pregnancy
- Difficult labour and delivery or childbirth trauma
- Being overweight or obese
- Lower oestrogen level after menopause
- Chronic constipation
- Chronic cough or bronchitis
- Repeated heavy lifting
- Major pelvic surgery requiring external support
Uterine prolapse diagnosis
The doctor will assess your symptoms and perform a pelvic examination. During the examination, the doctor may introduce a speculum to view the inside of the vagina, vaginal canal, and uterus.Treatment
If the prolapse is minor, there is no therapy. Non-surgical treatment for moderate-to-severe uterine prolapse may include:- Decreasing weight to relieve stress on pelvic tissues
- Avoid heavy lifting
- Doing Kegel exercises, which are pelvic floor exercises that strengthen the vaginal muscles
- Using a pessary, which is a vaginal device that fits beneath the cervix and helps in pushing up and stabilising the uterus and cervix.
- The benefits of vaginal oestrogen have been extensively researched, and results demonstrate an improvement in restoring vaginal strength and regeneration of vaginal tissue.
- The disorder can be treated surgically by uterine suspension or hysterectomy. Pelvic ligaments are reattached during uterine suspension to retain the uterus in its original place. The term “hysterectomy” refers to the surgical removal of the uterus through the vagina or abdomen.
- Though surgery is quite beneficial, it is not recommended for women who are still trying to conceive. Pregnancy and childbearing can impose enormous strain on pelvic muscles, potentially undoing uterine repairs.
Surgery
Hysterectomy and prolapse repair: Uterine prolapse can be repaired with a hysterectomy, which involves removing the uterus. This can be done via a cut (incision) in the vaginal canal (vaginal hysterectomy) or through the abdomen (abdominal hysterectomy) . Recovery time usually takes 1 week after surgery. Prolapse repair without surgery entails repositioning the uterus to its original position. The pelvic ligaments are reattached to the bottom section of the uterus to keep it in place during uterine suspension. Depending on the technique employed, the procedure might be performed through the vaginal or abdominal canals. The patient can be discharged from the hospital on the same day after treatment.Uterine prolapse complications
Other related organs may prolapse as a result of uterine prolapse.- Anterior prolapse (cystocele): The bladder may expand into the vagina due to a weakening in the connective tissue that separates the bladder and the vagina. Anterior prolapse is often referred to as a prolapsed bladder.
- Rectocele (posterior vaginal prolapse): The rectum may expand into the vagina due to a weakening in the connective tissue that separates the rectum and vagina. It may have an impact on your bowel movements.
Prevention
- Getting regular physical activity
- Maintaining a healthy weight
- Practicing Kegel exercises
- Seeking treatment for conditions that increase your pelvic pressure, such as chronic constipation or coughing
